Is Home Birth Safe?
 YES! Multiple large studies have shown that for healthy, low risk pregnancies in the care of a certified midwife, outcomes for women and babies are as good, if not better, than those with MD and hospital care (see resources).Throughout the course of pregnancy your midwife will monitor your well-being and your baby’s well being. It is possible for a pregnancy to become complicated by a number of factors before labor and your midwife will work with you to correct these factors and will collaborate with other care providers to manage the problem. In labor, you and your baby will be carefully monitored according to guidelines to maintain a safe and low risk birth. In the event of deviations from normal, your midwife will work with you and your birth team to make the proper decision and seek advanced care as necessary. Katie has a long standing relationship with the broader network of providers in the Duluth area and appreciates the ease of making referrals and collaborating with other doctors in the rare event that this is needed. She is well respected and supported by the local obstetrics community and Duluth hospitals.
YES! Multiple large studies have shown that for healthy, low risk pregnancies in the care of a certified midwife, outcomes for women and babies are as good, if not better, than those with MD and hospital care (see resources).Throughout the course of pregnancy your midwife will monitor your well-being and your baby’s well being. It is possible for a pregnancy to become complicated by a number of factors before labor and your midwife will work with you to correct these factors and will collaborate with other care providers to manage the problem. In labor, you and your baby will be carefully monitored according to guidelines to maintain a safe and low risk birth. In the event of deviations from normal, your midwife will work with you and your birth team to make the proper decision and seek advanced care as necessary. Katie has a long standing relationship with the broader network of providers in the Duluth area and appreciates the ease of making referrals and collaborating with other doctors in the rare event that this is needed. She is well respected and supported by the local obstetrics community and Duluth hospitals.
Is Home Birth Messy?
Not very! Your midwife will provide you with a birth supplies list and a birth kit that encompasses the essentials for labor and birth and useful things to clean and contain any potential messes. After your birth you and your new babe will be tucked into bed, laundry will be started or placed near your washing machine, the trash will be taken out, beds remade as needed and the birth area tidied up. It is important that you and your partner are able to rest after the birth. Most visitors will not be able to tell where you had your baby in your home.
Can I have a doula?
Absolutely! We love working with doulas! A common misconception is that doulas and midwives do the same things. While there are areas of overlapping support, this is incorrect. Doulas are a specially trained labor coach, not a health care provider. They meet with you a few times prenatally to help you prepare for labor and birth and teach you comfort measures for labor. A doula provides emotional support and comfort measures for moms and partners throughout labor and has no medical responsibility. Midwives are your health care providers. Midwives are trained and certified in resuscitation, can administer medications, listen to your baby’s heartbeat, check your vitals and perform cervical exams. Attentive labor support is the hallmark of what midwives do! Midwives are skilled at providing emotional and physical support to laboring women and will also have their hands busy with monitoring the progress of labor and vital signs so we welcome having a doula on your birth team as well. Doulas are especially helpful in the early stage of labor when you are in need of support and it is not yet time for your midwife to remain with you.
 What are my pain management options?
What are my pain management options?
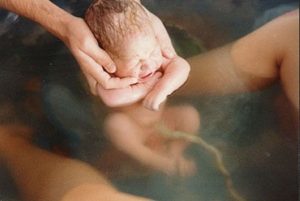
At home births, the pain management options are much more natural than in a hospital. There are no pharmaceutical pain medication offered at home (i.e. an epidural or injections). Your midwife uses various ways to help you get through the hard work of labor and birth. We will suggest different positions, use massage, essential oils, movement, encourage breathing and relaxing, dancing, getting in the shower, using a birth tub and connecting with your partner and baby as methods to work with your labor pain or sensations. Women find that when their labor is unfolding naturally, in their own space surrounded by a supportive team they trust and know well, they are able to find their rhythm and work with their contractions naturally and without pain medications. We have spent hours together prenatally preparing you for the hard physical and emotional work of labor and birth. You and your partner will know what to expect and have trust in your body and birth and have confidence with your trusted midwife by your side.
What happens if we need to go to the hospital in labor?
The majority of the time that we transfer care into the hospital in labor it is non-urgent. The most common example of this would be a long labor that has become dysfunctional and is no longer progressing (contractions have become irregular or faded out) and the mom is exhausted. She may need pain management and medication for rest, or Pitocin (a medication to increase contractions). In this case, we, as a collective birth team, have tried many things and have been discussing the options to manage the problem and all feel hospital help is the best option. It is important to include the birthing mama and supportive partners in the decision to transfer. We would call ahead to the hospital, pack a bag, bring snacks and take your private car. Katie will bring your prenatal and labor records and will accompany you to transfer your care to the hospital provider. Our goal is to have one of your LSM birth team stay with you as your advocate and support. At this point Katie will no longer be your primary provider for your labor and birth.
It is rare that we transfer to a hospital in an urgent and rushed manner. Throughout your labor I Katie is monitoring for “pink flags” or signs that something is going amiss. We do not sit at home with too many “pink flags” and we do not wait for a big red flag. We make every effort to transfer sooner rather than later if we are anticipating more complications. Katie is committed to healthy outcomes for moms and babies. A few examples of why we might take an ambulance to a hospital include: a placenta that is not being born at home, severe issues with the baby’s heart rate in labor, or a baby with respiratory issues.
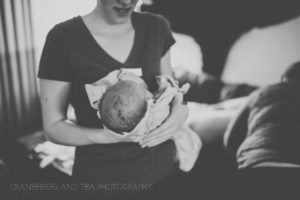
If a transfer of care occurs, you have the option and are encouraged to continue seeing Katie postpartum and newborn care when you return home. Katie will be available to discuss and process your labor and birth experience throughout your postpartum care.
How often are visits and when can I start?
 Prenatal visits typically start between 10-12 weeks gestation. By this point in pregnancy you may have had time to meet with several providers and choose the one that is the best fit for you. Some clients initiate care after they have had prenatal care with another provider, but many start with Katie. After the initial visit you are seen every 4-6 weeks until 28 weeks gestation, then every 2 weeks until 36 weeks. At 36 weeks you will have a home visit where Katie and the birth assistant will get oriented to your birth space, make sure you have all of your birth supplies and they know how to get to your home. After this home visit you will have prenatal visits in the office weekly until baby is born. Once your baby is born Katie will visit you at home at day one, day three and day seven. You will then return to the office for visits at 2 weeks and 6 weeks. Katie is on call for you from the initial prenatal visit until the final postpartum visit.
Prenatal visits typically start between 10-12 weeks gestation. By this point in pregnancy you may have had time to meet with several providers and choose the one that is the best fit for you. Some clients initiate care after they have had prenatal care with another provider, but many start with Katie. After the initial visit you are seen every 4-6 weeks until 28 weeks gestation, then every 2 weeks until 36 weeks. At 36 weeks you will have a home visit where Katie and the birth assistant will get oriented to your birth space, make sure you have all of your birth supplies and they know how to get to your home. After this home visit you will have prenatal visits in the office weekly until baby is born. Once your baby is born Katie will visit you at home at day one, day three and day seven. You will then return to the office for visits at 2 weeks and 6 weeks. Katie is on call for you from the initial prenatal visit until the final postpartum visit.
What if I don’t live in Duluth?
Not a problem! Katie attends births within 60-90 minutes of Duluth. If you have questions or concerns about midwifery care based on your location please contact the midwife to discuss your specifics.
What are the differences and similarities between a Certified Nurse Midwife and a Certified Professional Midwife?
A Certified Nurse Midwife (CNM) is a registered nurse (RN) with a bachelor’s degree and a postgraduate degree in midwifery. A CNM is an independent practitioner and expert in women’s health as well as maternity care and birth. She is a primary care provider for women. Their scope of practice allows them to be independent of doctors, prescribe medications, and may work in a clinic, hospital, or private practice including out of hospital birth in a home or birth center. They are certified nationally by the American College of Nurse Midwives (ACNM) and maintain their credentials through the American Midwifery Certification Board (AMCB) by meeting continuing education requirements. In Minnesota, CNM’s are licensed to practice by the Board of Nursing as an Advanced Practice Registered Nurse.
 A Certified Professional Midwife (CPM) is a person trained solely in out of hospital birth and maternity care. CPMs can practice in freestanding birth centers or home birth practices. They do not have the ability to write prescriptions or practice in hospitals. There are two educational paths that can be taken to become a CPM; apprenticeship or attendance at an accredited midwifery school. After completing their educational program, CPMs are certified through the National Registry of Midwives (NARM). Each state has different licensing requirements for CPMs. In Minnesota licensure is voluntary and in Wisconsin it is required.
A Certified Professional Midwife (CPM) is a person trained solely in out of hospital birth and maternity care. CPMs can practice in freestanding birth centers or home birth practices. They do not have the ability to write prescriptions or practice in hospitals. There are two educational paths that can be taken to become a CPM; apprenticeship or attendance at an accredited midwifery school. After completing their educational program, CPMs are certified through the National Registry of Midwives (NARM). Each state has different licensing requirements for CPMs. In Minnesota licensure is voluntary and in Wisconsin it is required.
Despite the difference in credentialing, CNMs and CPMs are very similar. Both are midwives who are experts in low risk pregnancy and out of hospital birth. CNM’s and licensed CPM’s follow similar guidelines and standards of care that are proven to promote good outcomes for pregnancy and birth. Unlicensed midwives may not follow those standards of care.
